Menu Requirements
Nutrition Requirements
- Dietary Guidelines
The Older Americans Act requires that meals comply with the current Dietary Guidelines for Americans (DGA) published by the Secretary of Health and Human Services and the Secretary of Agriculture.
Each participating older individual shall be provided with meals that meet nutritional standards. If the program provides:
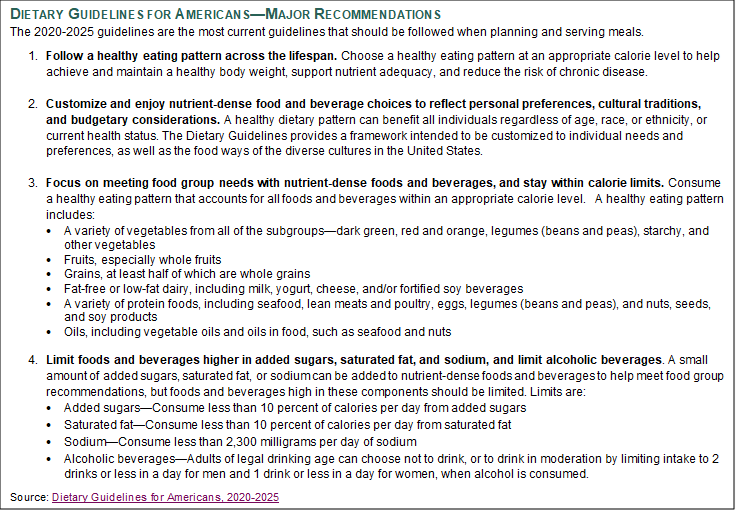
Source: Dietary Guidelines for Americans, 2020-2025
- Menu Requirements
The nutritional goals listed below represent the current DRI values, per meal and per day, for target nutrients to meet the DRI for a 51+ year old female which corresponds to 1600 calories per day.
|
Nutrient |
Source* |
Target per Day |
Target per Meal |
|
Calories (Kcal) |
AMDR |
1600 |
550 - 650 |
|
Protein (g) * |
RDA |
≥ 46 |
≥ 15 (from protein and dairy/soy alternative groups) |
|
Fat (% of total calories) |
AMDR |
20 - 35% |
20 - 35% |
|
Saturated Fat (% of total calories) |
DGA |
≤ 10% |
≤ 10% |
|
Fiber (gm) |
AI |
≥ 22 |
≥ 7 (weekly average) |
|
Calcium (mg) |
RDA |
≥ 1200 |
≥ 400 (weekly average) |
|
Magnesium (mg) |
RDA |
≥ 320 |
≥ 105 (weekly average) |
|
Potassium (mg) |
AI |
≥ 2600 |
≥ 860 (weekly average) ** |
|
Sodium (mg) |
AI and CDRR |
≤ 2300 |
≤ 760 (weekly average) |
|
Vitamin A (mcg RAE***) |
RDA |
≥ 700 |
≥ 233 (2 - 3 meals out of 5 meals per week) |
|
Vitamin D (IU) |
RDA |
600 |
200 (weekly average) |
|
Vitamin C (mg) |
RDA |
≥ 75 |
≥ 25 |
|
Vitamin B12 (mcg) |
RDA |
2.4 |
0.8 (weekly average) |
*AI = Adequate Intake, AMDR = Acceptable Macronutrient Distribution Range; CDRR = Chronic Disease Risk Reduction Level; DGA = Dietary Guidelines for Americans, 2020-2025; RDA = Recommended Dietary Allowance.
** Prior to 2019, the AI for K+ was 4700 (1565 per meal) but was updated in 2019 to 2600 (860/meal) for women and 3400 (1133 per meal) for men. Source: https://www.nap.edu/read/25353/chapter/8#120
*** RAE = Retinol Activity Equivalents
- Menu Analysis
Menus must be analyzed for nutritional adequacy and to ensure that the meals follow the DGA and provide a minimum of one-third of the DRI as required by the OAA and CCR Nutritional adequacy is based on standardized recipes and nutritional information published by the manufacturers for all menu items, including condiments. Nutritional information for fresh fruits and vegetables should be based on the type and amount to be served. All menus, and any substitutions, must be approved by a Registered Dietitian (RD). Menus may be analyzed using either the Computerized Nutrient Analysis or Meal Pattern Component.- Nutrient Analysis
Computerized nutrient analysis is the most accurate method for analyzing meals for nutritional adequacy. Meals are in compliance with requirements when they meet one-third of the DRI for target nutrients, provide an appropriate calorie level, and follow the Dietary Guidelines. The following nutrients must be included in the analysis: calories, protein, carbohydrates, total fat, saturated fat, total fiber, vitamins A, C, E, K, B1 (thiamin), B2 (riboflavin), B3 (niacin), B6 (pyridoxine), folate, B12 (cyanocobalamin), and minerals—calcium, chromium, copper, iron, magnesium, sodium, and zinc. In addition, the SNP requires nutrient analysis for vitamin D and potassium. - Meal Pattern Components
The meal pattern component serves as a basic framework for menu planning. Meals comply with requirements when food component guidelines and serving sizes are followed. The meal pattern component can be used to plan NMOW meals. A template can be found in Appendix: Summary of Menu Requirements for Meal Pattern Component and a summary of the requirements can be found in Appendix: Summary Menu Requirements 2022. NMOW contractor shall follow key nutrients outlined in Meal Planning Requirements including the following:- Kilocalories
- Menus shall provide an average of at least 533 kilocalories (kcal) per meal.
- Protein – Meat, Fish, Poultry, Legumes, Eggs and Cheese
- The meal shall contain a minimum of 3 ounces (per County) of cooked, edible portions of meat, fish, seafood, poultry, legumes, beans, peas, soy products, nuts, seeds, eggs, cheese OR a combination thereof providing at least 15 grams of protein.
- Mixed main entrees such as casseroles, pastas and entrée salads should provide at least 15 grams of protein.
- Use legume dishes (using mature dried beans such as lima, kidney, navy, black, pinto or garbanzo beans, lentils, peas, black eyed peas and soybeans) as often as possible in accordance with participants’ acceptance.
- Legume dishes should not be counted as both a vegetable and a protein in the same meal.
- Alternate protein sources are healthy options to include in the menu. The SNP recommends at least one vegetarian meal per week. A list of lean and healthy protein sources is found in Appendix: Lean Healthy Protein Sources.
- Portion controlled items and other convenience foods (e.g. fish fillet, pork chop, stuffed peppers and cabbage, lasagna, or chile relleno) must contain no more than 480 mg. sodium per serving. (County guideline).
- Extra lean beef and pork (total fat ≤ 5%) and at least 90% lean ground beef is recommended.
- The County recommends the use of lean ground meat in entrees no more than twice a week. If served twice in one week, the ground meat shall be served at least once in “solid” form such a meat loaf or Salisbury steak.
- Imitation cheese cannot be served as meat alternates.
- Breads/Grains
- Each meal shall contain one to two servings of grain. One serving must be whole grain.
- Bread, cereal, and baked items must contain less than 215 mg sodium per serving.
- Cereal shall contain less than 6 gm sugar per serving.
- A variety of whole grain products should be consumed. Those highest in fiber are recommended: barley, brown rice, bulgur, dried ground corn (cornmeal, masa), oats, quinoa, whole rye, whole wheat and wild rice.
- A list of whole grain foods is found in Appendix: Whole Grains.
- Vegetables
- Each meal shall contain at least 1 to 2 servings of vegetables, drained weight or volume of vegetables. (1/2 cup = 1 serving).
- Raw leafy vegetables must equal 1 cup per serving.
- Use fresh or frozen vegetables 3 – 4 times per week (60 – 80%). Minimize use of canned products. If canned vegetables are used, a serving should contain no more than 290 mg sodium.
- Vegetables as a primary ingredient in soups, stews, casseroles or other combination dishes must total ½ cup per serving (in order to be counted as a vegetable serving).
- Potatoes, sweet potatoes, yams and corn are considered as vegetables, not bread/grain.
- Legume dishes should not be counted as both a vegetable and a protein in the same meal.
- Fruits
- Each meal shall contain at least 1 serving of fruit. A serving of fruit is generally:
- Medium sized whole fruit (i.e. the size of a tennis ball); OR
- 2 – Small sized whole fruits; OR
- ½ cup fresh, chopped, cooked, frozen or canned, drained fruit; OR
- ½ cup 100% fruit juice.
- Serve fresh or frozen fruit at least 3 times per week.
- Canned fruit should be packed in juice, light syrup or without sugar.
- Fruit may be used as a fruit serving and a dessert in the same meal.
- Each meal shall contain at least 1 serving of fruit. A serving of fruit is generally:
- Milk and Approved Milk Substitutes
- Each meal shall contain eight (8) ounces of fortified (Vitamin A & D) skim (fat free), lowfat milk, lactose-free milk, or buttermilk (maximum of 1% milk fat). An equivalent substitute shall be served, such as an eight (8) ounces of calcium fortified soy milk, calcium fortified orange juice, or low-fat yogurt.
- According to Santa Clara County Nutrition Standards, flavored milk, such as vanilla or chocolate shall not be served. Calcium fortified plant derived milk such as soy, rice, or almond shall contain ≤130 calories per 8 oz. serving.
- All milk and approved milk substitute products shall be pasteurized.
- Fat
Fat is not a requirement. However, each meal may contain fat components to increase the palatability or acceptability of the meal. Healthy fats should be used in food preparation or served as an accompaniment to the meal when appropriate.
Fats and oils are part of healthful diet, but the type of fat makes a difference to heart health and the total amount of fat consumed is also important. Limit intake of fats and oils high in saturated fats and choose products low in such fats and oils. Products with trans-fatty acids may not be used or served.- Consume less than 10 percent of calories from saturated fatty acids and less than 300 mg/day of cholesterol.
- Keep total fat intake between 20 to 35 percent of calories, with most fats coming from sources of polyunsaturated and monounsaturated fatty acids, such as fish, nuts, and vegetable oils such as olive and canola oils.
- When selecting and preparing meat, poultry, and milk or milk products, make choices that are lean, low-fat or fat-free.
- Limit intake of fats and oils high in saturated and/or trans-fatty acids, and choose products low in such fats and oils.
- Shortening, lard, butter or other hydrogenated fats are not to be used in cooking or offered with the meal.
- Dessert
- Dessert is OPTIONAL but may be served no more than one time per week.
- Use fruit as a dessert as often as possible, limit sweets.
- Consider serving smaller portions of desserts such as cookies, cakes and other baked goods.
- Angel food cake, sorbet and frozen 100% juice bars are specifically considered by the County as acceptable desserts.
- Desserts that are low in fat or low in sugar are encouraged.
- When a dessert contains ½ cup of fruit per serving, it may be counted as a serving of fruit.
- Condiments
- Traditional meal condiments can be served as appropriate, e.g. tartar sauce with fish, mustard and mayonnaise with a meat sandwich, salad dressing with tossed salad, margarine with bread and rolls.
- Salt substitutes shall not be provided.
- Sugar substitutes, pepper, herbal seasonings, lemon, vinegar, non-dairy coffee creamer, salt and sugar may be provided but should not be counted as fulfilling any part of the nutritive requirements.
- Sodium
The commitment to reduce sodium in the meals stems from the fact that nutrition related chronic diseases remain the primary cause of death among people aged 65 and older. California has a diverse population, and the Elderly Nutrition Programs (ENPs) in the State provide culturally appropriate meals for many ethnicities.- The recommended sodium for each NMOW entree is less than 700 mg.
- The maximum amount of sodium allowed for an individual meal is 1200 mg.
- Meals that have more than 1000 mg sodium on the menu must state: “This meal contains more than 1000 mg of sodium” or be identified with an icon noting that it is a high sodium meal.
- For all cuisines:
- Use only low sodium versions of high sodium foods and seasonings (such as salad dressings, gravies, soup bases, soy sauce) when available and feasible within budget allowances.
- Use of low sodium items wherever possible assuming cost neutrality.
- Omit salt in a recipe or be limited to ¼ or less than the amount required.
- Use herbs, spices and seasonings without added salt.
- Rinse food items packaged with sodium as a preservative (e.g. beans or tuna).
- Iodized salt should be used in cooking or when made available to clients.
- Use low sodium soy sauce or diluting soy sauce with water to produce low sodium soy sauce.
- Refrain from using food items such as raw chicken with sodium preservatives. Base Reference for Sodium Content of Commonly Served Foods in the SNP can be found in Appendix: Base Reference Sodium Content.
- Other nutrients of special importance:
- Vitamin A
- A Vitamin A rich food shall be served at least one (1) time per week for a three (3) days a week menu, two (2) times per week for a four (4) days a week menu, three (3) times per week for a five (5) days a week menu and four (4) times per week for a seven (7) days a week menu.
- A Vitamin A rich food is a single serving or a combination of servings in the same meals that contains a minimum of 233 µg (retinol equivalents).
- A list of Vitamin A rich foods is found in Appendix: Vitamin A Vegetables and Fruits.
- Vitamin C
- A Vitamin C rich food or vegetables will be served daily and will provide 1/3 of the DRI or 25 mg each meal.
- A vitamin C rich food is a single serving or a combination of servings at the same meal.
- A list of Vitamin C rich foods is found in Appendix: Vitamin C Vegetables and Fruits.
- Fiber
- A weekly average of seven grams of fiber per meal can be met by including high fiber foods such as whole grains, vegetables, fruits, beans, peas, lentils, nuts and seeds.
- Calcium and Vitamin D:
- Provide a calcium-rich food at each meal, such as: Milk, yogurt, and fortified soy beverages.
- Dietary sources of Vitamin D include: Seafood and foods that are fortified with Vitamin D, including milk and fortified soy beverages.
- Modified Therapeutic Meals
Nutrition service providers may furnish modified meals where it is feasible, appropriate, and cost effective to meet the particular dietary needs that arise from religious or ethnic background or for the health needs of the participants. Meals for participants who require therapeutic diets may be offered only when the modified meal can be obtained from a facility where a registered dietitian-nutritionist approves the meals. - Modified Texture Meals
Modifying food texture and consistency may help older adults with chewing and swallowing problems. Chopping, grinding, pureeing or blending foods are common ways to modify food textures. Texture modified food has the same nutritive value of solid foods and it can be just as tasty and appealing. Serving size should account for any dilution to the food items during preparation. The provision of such foods should be planned and approved by the county registered dietitian nutritionist. - Food Allergens
CalCode section 113947 requires the “person in charge” and all food employees to have adequate knowledge of food safety as it relates to their assigned duties. The person in charge shall comply with both of the following:- Have adequate knowledge of major food allergens, food identified as major food allergens, and the symptoms that a major food allergen could cause in a sensitive individual who has an allergic reaction.
- Educate the employees regarding the information by using a poster or job aid to which the employee can refer.
- Supplements
- Vitamin and/or mineral supplements shall not be provided. Medical foods and food for special dietary uses shall not be provided with federal or state nutrition funds.
- Ethnic Meals
- Provide authentic ethnic cuisine, if applicable.
- Introduce new foods to coincide with ethnic and religious holidays.
- Offer variety of meals and/or foods from different ethnic groups.
- Vitamin A
- Kilocalories
- Nutrient Analysis
Menu Planning and Approval
Menu cycles start and end dates are based on calendar dates and will change slightly each fiscal year. Draft menus and/or corresponding nutritional analysis are due to the County two (2) months prior to the start of each cycle. Menus are finalized by the County for distribution two (2) weeks prior to the start of each cycle. All menus shall be approved by County registered dietitian. Food substitutions to meals originally planned must meet menu requirements and be approved by SNP registered dietitian. Client Facing Menu must be submitted to SNP on a monthly basis. A copy of this menu shall be provided to all registered clients.
Taste Test of Meals
SNP will conduct Taste Test of NMOW meals once annually or more often, if needed. The goal of the Taste Test is to evaluate the quality and acceptability of NMOW meals.
- Upon request, MOW provider will provide sample meals for Taste Test.
- Taste Test may be conducted at the NMOW provider facility, SNP office, or any selected location
- Upon completion, results of Taste Test will be shared with NMOW provider.
- NMOW provider shall change the menu item and/or recipe to meet the meal quality and acceptability requirement.